A joint is the area where two bones meet. Cartilage normally protects a joint, allowing it to move smoothly. Cartilage also absorbs shock when pressure is placed on the joint, such as when you walk. Without the normal amount of cartilage, the bones rub together, causing pain, swelling (inflammation), and stiffness. Arthritis is inflammation of one or more joints and also involves the breakdown of cartilage.
- An autoimmune disease (the body's immune system mistakenly attacks healthy tissue)
- Broken bone
- General "wear and tear" on joints
- Infection, usually by bacteria or virus
Usually the joint inflammation goes away after the cause goes away or is treated. Sometimes it does not. When this happens, you have chronic arthritis. Arthritis may occur in men or women.
The common types of arthritis include the following:
Osteoarthritis not resulting from injury or disease, is mostly a result of natural aging of the joint. With aging, the water content of the cartilage increases, and the protein makeup of cartilage degenerates. Eventually, cartilage begins to degenerate by flaking or forming tiny crevasses. In advanced osteoarthritis, there is a total loss of the cartilage cushion between the bones of the joints. It is mainly related to aging. The symptoms of OA usually appear in middle age. Almost everyone has some symptoms by age 70. However, these symptoms may be minor. Before age 55, OA occurs equally in men and women. After age 55, it is more common in women.
Other factors can also lead to OA.
- OA tends to run in families
- Being overweight increases the risk of OA in the hip, knee, ankle, and foot joints
- Fractures or other joint injuries can lead to OA later in life
- Long-term overuse at work or in sports can lead to OA
Symptoms
The pain of osteoarthritis typically begins gradually after age 40 and progresses slowly over many years. Younger people with the condition may have no symptoms at all. Osteoarthritis is commonly identified by the following symptoms:
- Pain that worsens during activity and gets better during rest. This is the most common symptom of osteoarthritis. As the disease advances, the pain may occur even when the joint is at rest.
- Pain is generally described as aching, stiffness, and loss of mobility. The symptoms are often worse when resuming activities after periods of no activity.
- The pain may be intermittent, with bad spells followed by periods of relative relief.
- Pain seems to increase in humid weather.
- Some people have muscle spasm and contractions in the tendons.
- Some people feel a grating sensation when the joint is used. Osteoarthritis in the knee may cause a crackling-like noise (called crepitus) when the affected knee is moved.
Treatment
Osteoarthritis itself is not life threatening, but a person''s quality of life can significantly deteriorate as a result of pain and lost mobility. No treatment can cure osteoarthritis, and none can alter its progression with certainty, but many available treatments can relieve symptoms and significantly improve the quality of life.
The goals of osteoarthritis treatment are to reduce pain and improve joint function. Treatment approaches include:
Lifestyle Changes - Exercise helps maintain joint and overall movement. Ask your health care provider to recommend an appropriate home exercise routine. Water exercises, such as swimming, are especially helpful.
Other lifestyle recommendations include:
- Applying heat and cold
- Eating a healthy, balanced diet
- Getting rest
- Losing weight if you are overweight
- Protecting the joints
- As the pain from your hip or knee OA becomes worse, keeping up with everyday activities may become more difficult or painful.
- Sometimes making changes around the home will take some stress off your joints, and relieve some of the pain.
- People whose work is causing stress in certain joints should find ways to reduce trauma. You may need to adjust your work area or change work tasks.
Medications - For mild pain relief, doctors recommend acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), and topical ointments. Patients with more severe pain may require stronger narcotic pain medication, corticosteroid injections, or visco-supplementation with injections of hyaluronic acid drugs.
Surgery - For severe osteoarthritis that is not helped by other treatments, surgery such as joint replacement may be considered. Severe cases of OA might need surgery to replace or repair damaged joints. Surgical options include:
- Arthroscopic surgery to trim torn and damaged cartilage
- Changing the alignment of a bone to relieve stress on the bone or joint (osteotomy)
- Surgical fusion of bones, usually in the spine (arthrodesis)
- Total or partial replacement of the damaged joint with an artificial joint (knee replacement, hip replacement, shoulder replacement, ankle replacement, elbow replacement)
Ankylosing spondylitis is a long-term disease that causes inflammation of the joints between the spinal bones, and the joints between the spine and pelvis. It eventually causes the affected spinal bones to join together.
Symptoms
The disease starts with low back pain that comes and goes.
- Pain and stiffness are worse at night, in the morning, or when you are not active. It may wake you from your sleep.
- The pain typically gets better with activity or exercise.
- Back pain may begin in the sacroiliac joints (between the pelvis and the spine). Over time, it may involve all or part of the spine.
You may lose motion or mobility in the lower spine. You may not be able to fully expand your chest because the joints between the ribs are involved.
Fatigue is also a common symptom.
Other symptoms include:
- Eye inflammation
- Heel pain
- Hip pain and stiffness
- Joint pain and joint swelling in the shoulders, knees, and ankles
- Loss of appetite
- Slight fever
- Weight loss
Gonococcal arthritis is inflammation of a joint (usually just one) due to a gonorrhea infection. Gonococcal arthritis is an infection of a joint. It occurs in people who have gonorrhea caused by the bacteria Neisseria gonorrhoeae.
If the infection spreads to the bloodstream, fever, rash, and arthritis-like symptoms may occur. It affects women more often than men, and it is most common among sexually active adolescent girls.
If the infection spreads to the bloodstream, fever, rash, and arthritis-like symptoms may occur. It affects women more often than men, and it is most common among sexually active adolescent girls.
Two forms of gonococcal arthritis exist:
- One involves skin rashes and many joints, usually large joints such as the knee, wrist, and ankle
- The second, less common form involves the spread of the bacteria through the blood (disseminated gonococcemia), which leads to infection of a single joint
Gouty arthritis is a common cause of a sudden onset of a painful, hot, red, swollen joint, particularly in the foot at the big toe. Gouty arthritis is reportedly the most common cause of inflammatory arthritis in men over the age of 40.
It is definitively diagnosed by detecting uric acid (monosodium urate) crystals in an aspirated sample of the joint fluid. These uric acid crystals can accumulate in the joint and tissues around the joint over years, intermittently triggering repeated bouts of acute inflammation. Repeated "attacks" of gouty arthritis, or "flares," can damage the joint and lead to chronic arthritis.
It is definitively diagnosed by detecting uric acid (monosodium urate) crystals in an aspirated sample of the joint fluid. These uric acid crystals can accumulate in the joint and tissues around the joint over years, intermittently triggering repeated bouts of acute inflammation. Repeated "attacks" of gouty arthritis, or "flares," can damage the joint and lead to chronic arthritis.
Treatment
Self-Care at Home
- Take medications as prescribed.
- While a joint is hot and swollen, you may want to use a cane or similar support to keep your weight off that joint.
- It may be helpful to keep the swollen joint elevated above your chest as much as possible.
- Ice packs can be helpful in relieving pain and reducing inflammation.
- Maintaining adequate hydration is key for minimizing the frequency and intensity of attacks.
- Cherry juice may decrease the intensity and severity of attacks.
If you are at risk for gout, you should do the following:
- Eat a low-cholesterol, low-fat diet. People with gout have a higher risk for heart disease. This diet would not only lower your risk for gout but also your risk for heart disease. Control your cholesterol.
- Avoid foods that are high in purines (the biochemical in foods that is metabolized into uric acid), including shellfish and red meats.
- Slowly lose weight. This can lower your uric acid levels. Losing weight too rapidly can occasionally precipitate gout attacks.
- Restrict your intake of alcohol, especially beer.
- Stay hydrated.
- Increase your intake of dairy products, such as nonfat milk and yogurt, because they can lower the frequency of gout attacks.
- Avoid fructose, such as in corn syrup.
- Talk to your doctor if you are taking thiazide diuretics (HCTZ), low-dose aspirin, levodopa (Larodopa), cyclosporine (Gengraf, Neoral, Sandimmune), or nicotinic acid.
Juvenile rheumatoid arthritis, also known as juvenile idiopathic arthritis, is the most common type of arthritis in children under the age of 16. Juvenile rheumatoid arthritis causes persistent joint pain, swelling and stiffness. Some children may experience symptoms for only a few months, while others have symptoms for the rest of their lives.
Some types of juvenile rheumatoid arthritis can cause serious complications, such as growth problems and eye inflammation. Treatment of juvenile rheumatoid arthritis focuses on controlling pain, improving function and preventing joint damage.
It is divided into several types:
- Systemic (bodywide) JRA involves joint swelling or pain, fevers, and rash. It is the least common type.
- Polyarticular JRA involves many joints. This form of JRA may turn into rheumatoid arthritis. It may involve five or more large and small joints of the legs and arms, as well as the jaw and neck.
- Pauciarticular JRA involves four or less joints, most often the wrists, or knees. It also affects the eyes.
Symptoms
Symptoms of JRA may begin with a swollen joint, limping, a spiking fever, or a new rash.
Symptoms can include:
- Joint stiffness and pain
- Limited range of motion
- Warm, swollen, or red joints
- A child may stop using an affected limb or may limp
Body-wide JRA symptoms:
- Fever, usually high fevers every day
- Rash (trunk and extremities) that comes and goes with the fever
- Pale skin
- Looks sick
- Swollen lymph nodes (glands)
JRA can also cause eye problems red eyes, eye pain which may get worse when looking at light
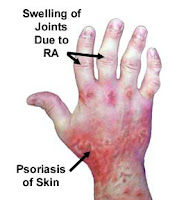
Psoriatic arthritis is a type of arthritis that often occurs with psoriasis of the skin.
Causes
Psoriasis is a common, chronic skin condition that causes red patches on the body. About 1 in 20 people with psoriasis will develop arthritis with the skin condition. In most cases, psoriasis comes before the arthritis.
The cause of psoriatic arthritis is not known, but genes may play a role. In general, people who have psoriasis have a higher rate of arthritis than the general population.
Symptoms
The arthritis may be mild and involve only a few joints, particularly those at the end of the fingers or toes. In some people the disease may be severe and affect many joints, including the spine. When the spine is affected, the symptoms are stiffness, burning, and pain, most often in the lower spine and sacrum.
People who also have arthritis usually have the skin and nail changes of psoriasis. Often, the skin gets worse at the same time as the arthritis.
Rheumatoid arthritis (RA) is a long-term disease that leads to inflammation of the joints and surrounding tissues. It can also affect other organs.
Causes
The exact causes of rheumatoid arthritis are unknown. Rheumatoid arthritis is most likely triggered by a combination of factors, including an abnormal autoimmune response, genetic susceptibility, and some environmental or biologic trigger, such as a viral infection or hormonal changes.
The Normal Immune System Response and inflammatory process
- The inflammatory process is a byproduct of the activity of the body's immune system, which fights infection and heals wounds and injuries:
- When an injury or an infection occurs, white blood cells are mobilized to rid the body of any foreign proteins, such as a virus.
- The masses of blood cells that gather at the injured or infected site produce factors to repair wounds, clot the blood, and fight any infections.
- In the process the surrounding area becomes inflamed and some healthy tissue is injured. The immune system is then called upon to repair wounds by clotting off any bleeding blood vessel and initiating fiber-like patches to the tissue.
- Under normal conditions, the immune system has other special factors that control and limit this inflammatory process.
Symptoms
RA usually affects joints on both sides of the body equally. Wrists, fingers, knees, feet, and ankles are the most commonly affected.
The disease often begins slowly, usually with only minor joint pain, stiffness, and fatigue.
Joint symptoms may include:
- Morning stiffness, which lasts more than 1 hour, is common. Joints may feel warm, tender, and stiff when not used for an hour.
- Joint pain is often felt on the same joint on both sides of the body.
- Over time, joints may lose their range of motion and may become deformed.
Other symptoms include:
- Chest pain when taking a breath (pleurisy)
- Dry eyes and mouth (Sjogren syndrome)
- Eye burning, itching and discharge
- Nodules under the skin (usually a sign of more severe disease)
- Numbness, tingling, or burning in the hands and feet
Treatment
RA usually requires lifelong treatment, including the following:
Medications
Physical therapy - Range-of-motion exercises and exercise programs prescribed by a physical therapist can delay the loss of joint function and help keep muscles strong.
- Sometimes therapists will use special machines to apply deep heat or electrical stimulation to reduce pain and improve joint movement.
- Joint protection techniques, heat and cold treatments, and splints or orthotic devices to support and align joints may be very helpful.
- Frequent rest periods between activities, as well as 8 to 10 hours of sleep per night, are recommended.
Exercise
Patient and family education
Possibly surgery - Surgery may include:
- Removal of the joint lining (synovectomy)
- Total joint replacement in extreme cases; may include total knee, hip replacement, ankle replacement, shoulder replacement, and others
Early, aggressive treatment for RA can delay joint destruction.
Also Read:-